By Justin Hsieh

The COVID-19 pandemic has sickened over 200,000 people in more than 140 countries and killed over 8,000. Governments and communities scrambling to contain or prevent the disease’s transmission have implemented measures designed to limit large congregations of people, from canceling concerts and competitions to closing schools and restaurants.
What has become increasingly clear, however, is that the best method of getting this pandemic under control depends on all of us. Social distancing, or minimizing contact with other people on a voluntary and individual basis, is the key to saving lives and preventing suffering in the face of this extraordinary public health crisis.
The purpose of social distancing is to limit the number of person-to-person interactions by which an infectious disease may be spread. By limiting nonessential travel, skipping social gatherings, working from home and avoiding public transportation, we give this coronavirus fewer opportunities to infect healthy people and we slow its spread as much as possible.
Yet for some young people, many of whom are less likely to develop severe symptoms in the event of infection and are used to frequent social gathering, public health officials’ calls for self-isolation and social distancing seem restrictive, unappealing and unnecessary. Does it really matter if healthy young people hang out with their friends?
The answer, crucially, is yes. A categorical, emphatic yes.
The reason for this is that social distancing is as much about preventing a person from contracting an infectious disease (like COVID-19) as it is preventing them from transmitting it to others. It’s meant to protect people who are not as young or healthy, including the elderly and people of all ages who have underlying health conditions or are immunocompromised.
Social distancing doesn’t just protect you. If you live with your grandparents, it protects them. If you know someone who lives with their grandparents, it protects them. If you have a family member with a heart problem, it protects them. If your friend has a family member with a heart problem, it protects them.
Vulnerable patients may be the ones the coronavirus hurts the most, but healthy individuals are the ones it relies on to get to them. That’s why every social interaction that doesn’t happen is one fewer opportunity for you to unknowingly take home a virus and give it to your family, or to bring a virus with you and pass it on to someone else.
This is especially important because of the nature of this coronavirus. Many people compare the virus responsible for COVID-19 to the one that causes seasonal flu and argue that because we don’t take extreme measures to combat influenza, they aren’t necessary here. But that argument misses several key differences between COVID-19 and the flu.
For one, COVID-19 is considerably more contagious than the flu. The basic reproduction number (R0), the number of people that an average infected person can be expected to infect, is up to 2 times higher than that of the flu (2-2.5 for COVID-19 compared to 1.3 for the flu).
COVID-19 is also more dangerous than the flu. The hospitalization rate is almost ten times higher (19% compared to 2%), and even the lowest observed death rates (0.2% in Germany, where more extensive testing and preparation was done than in the U.S.) have been double that of the flu, which averages around 0.1% or lower. Other estimates from the CDC and WHO put the mortality rate of COVID-19 somewhere between 1-3.4%.
The high infectiousness and severity of COVID-19 merit atypical measures to contain its spread and protect the vulnerable. What’s even more important is that COVID-19 can have an incubation period (time after infection before symptoms) up to two weeks longer than that of the flu, and that no vaccine currently exists for the disease (realistic estimates put the timeline for development, testing, approval and mass production of a vaccine in mid-2021).
These factors mean that it’s significantly easier for people to catch and transmit COVID-19, even if they don’t have symptoms and don’t know they are infected. Every young person, regardless of how healthy they feel, could be carrying the virus and spreading it into the air and onto surfaces around them (where it can live for up to 3 days, given the right conditions) without knowing. Every unnecessary social outing, therefore, is a gamble with other people’s health.
The importance of social distancing extends beyond its impacts on people in our immediate communities. Social distancing is a critical part of a larger societal effort to slow the spread of COVID-19 so that it doesn’t overwhelm the capacity of the healthcare system.
Current estimates already show that the country has a critical shortage of ventilators and hospital beds to handle an influx of COVID-19 patients. Only so many people can use those ventilators and beds at once, and if more people come into a hospital than it can handle at any given time some people will be forced to go without.
If that does occur, the fatality rate of the disease will increase as people who could be saved go untreated and die because there are not enough resources to treat them or keep them alive. Even patients who don’t have COVID-19, but who go to the hospital for other critical health needs, could suffer or die in the face of hospital bed and care shortages.
This is a very real possibility. It happened in Italy, where a massive influx of cases all at once exceeded hospital capacities and forced doctors to choose which patients to save, leaving the patients least likely to recover to die and focusing their limited resources on the patients with the best chance of success. In some cases, doctors considered establishing an age limit for access to intensive care, following the cruel logic that older patients would have fewer “life-years” left than younger patients even if they did survive.
It also happened 100 years ago in Philadelphia, when in the face of the H1N1 virus (commonly referred to as the Spanish flu) the city neglected to cancel a 200,000-person parade. Within 72 hours, every hospital bed in the city was filled, and by the end of the week 2,600 people in the city had died.
That is what will happen if we cannot control this virus. At some level, the question of if you will be infected with COVID-19 is less important than when. The later that is, the better. If we take no precautions and allow the virus to spread as quickly as it can, everyone will be infected at once, hospitals will be flooded and people who could live will die.
On the other hand, if we stay home, stay away from others and are as vigilant as possible in keeping ourselves and everyone around us healthy, we can slow the spread of COVID-19 to a crawl. Even if the same number of people get infected, it’ll happen over a much longer period of time and the number of simultaneous infections will never be as high as in the case of uncontrolled transmission. In this case, we keep care open and available for those who need it and make sure that nobody suffers or dies when they don’t have to.
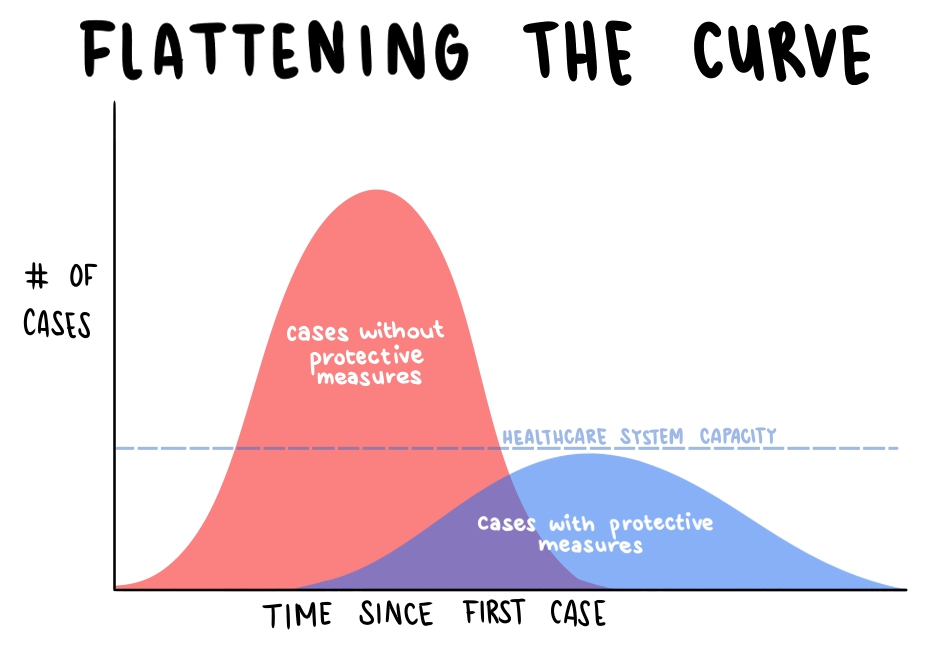
Slowing the rate of infection is called ‘flattening the curve,’ and it’s the goal behind recent measures like the CDC’s recommendation against gatherings of over 10 people or Orange County’s restriction against gatherings of any kind outside immediate living units. These measures, though, only work if everyone follows them.
And follow them we must. It is our moral duty in this time of crisis. Science and history tell us that social distancing saves lives and prevents suffering, and that it only works if all of us make the sacrifices demanded of us. So stay home. Seriously.
*Note: “staying home” and social distancing refer to limiting contact with other people. Experts and officials say going outside for fresh air and for essential activities like buying food and medicine are fine, as long as appropriate 6-ft distances between other people are observed.





